At Certilytics, we get it. We’ve spent our careers in population health and understand the challenges you face aligning your clinical outreach strategies with financial incentives.
Below are five tips we’ve learned first-hand through our experience helping some of the nation’s largest healthcare organizations and employers succeed in value-based care.
1) Risk Must Be Evaluated Across Benefits
The importance of cross-benefit health management has become more significant due to the substantial increase in pharmacy spend as a proportion of total healthcare costs. Payers have recognized the need for their care management programs to manage a member’s total health—not just medical utilization or drug compliance. The challenge however, is understanding how impacting utilization of one benefit (e.g., drug compliance) affects utilization on the other (e.g., reduced ER visits).
With the CORE® clinical episode grouper, Certilytics organizes member data—including clinical services and drug utilization—into a complete picture of member health, allowing our customers the ability to “connect the dots” and point to the tangible benefit of their activity on each member’s total healthcare costs.
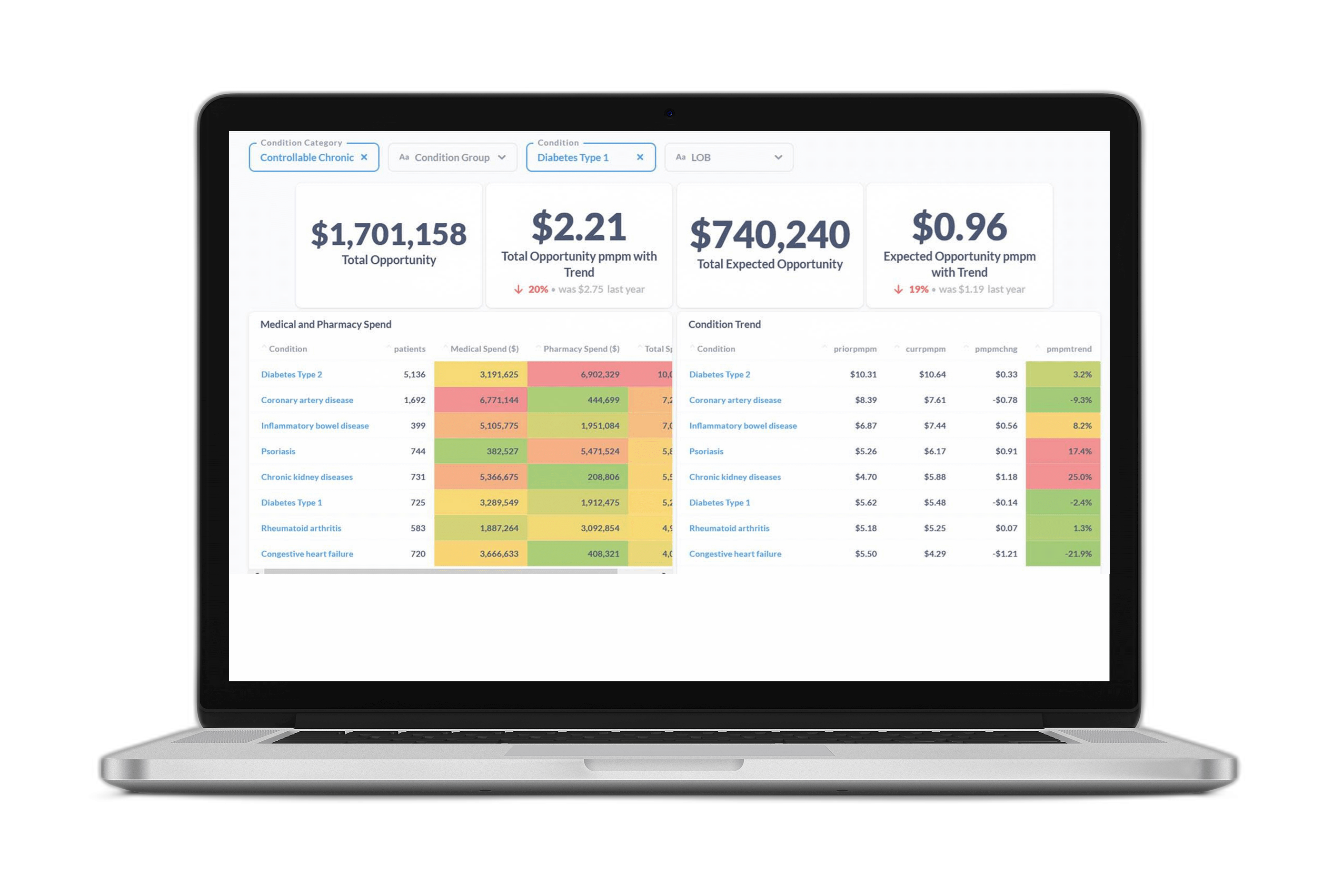
2) Balance Retrospective Utilization Against Forecasted Opportunity
When deciding who to prioritize for clinical intervention, it’s tempting to focus on the members with the highest utilization rates. After all, these members have a history of driving a disproportionate amount of your spend.
However, in order to bend the cost curve, it’s just as important that you understand your emerging risk and impact members before they incur exorbitant costs. For example, the clinical risk models don’t just look backward at a member’s utilization—but also forward at how likely each member is to utilize healthcare services in the future. This includes predicting members who will develop chronic conditions, or who already have a condition that hasn’t yet been diagnosed—enabling earlier interventions to prevent or better manage these conditions.
3) Clinical Outreach Strategy Must Align with Financial Goals
Every clinician’s top priority is improving member health outcomes—and rightfully so. However, many of the risk stratification tools traditionally used by clinicians differ from the tools used by actuaries and underwriters in their evaluation of risk. As payers take on new forms of risk based on the way their organizations manage total healthcare costs, it’s important that their clinical and financial constituencies are aligned so they receive credit (i.e., are reimbursed) for their activity.
Certilytics helps create alignment through the Opportunity Framework, which directly and transparently ties clinical outcomes to financial opportunities. This transparent and intuitive model attaches financial value to the mitigation of negative outcomes so that all stakeholders understand the value of steering members toward high value providers, closing gaps in care, enabling earlier interventions for those with emerging chronic conditions, and avoiding high-cost events.
4) Maximize Member Behavior Through Multi-Modal Outreach
A risk stratification tool that perfectly identifies the riskiest members isn’t worth anything unless a care manager can connect with members and get them to take action. In our experience, the most successful organizations employ a multi-modal approach to outreach—telephonic, digital, and provider-centric. Whatever risk stratification tool you use, make sure it can inform outreach through a variety of outreach modalities.
Certilytics solutions are designed not just to drive better population health management—but to measure the results. We can tell you which modalities are most effective, and which members are most likely to engage with a care management plan. Using our engagement model, one national insurer found that members identified as highly likely to engage were 2.6 times likelier to change their behaviors as a result of clinical outreach.
5) Proactive, Transparent, and Timely Performance Reconciliation is Critical
Due to the sheer magnitude of potential confounding factors, discerning the retrospective value of any clinical program is hard—especially when evaluating savings across benefits. In our experience, few organizations do this well. That’s why it’s important for your organization to have a transparent and timely method for tracking program performance—during and after implementation. Indeed, when multiple third-party managers are vying to take credit for affecting positive outcomes—the vendor with the most timely and understandable will win.
With Certilytics, you won’t just save money—you’ll understand exactly why you’re saving money and have the full support from our team of industry experts.