- A national insurer is using Certilytics products to optimize its care management programs, resulting in millions of dollars in potential year-over-year savings
- With Certilytics, the insurer saw a change in utilization patterns away from high-cost inpatient admissions toward lower-cost preventive services utilized on an outpatient basis or through a Primary Care Physician (PCP)
- The insurer found that patients identified as highly likely to engage by Certilytics were 2.6 times likelier to respond to clinical outreach
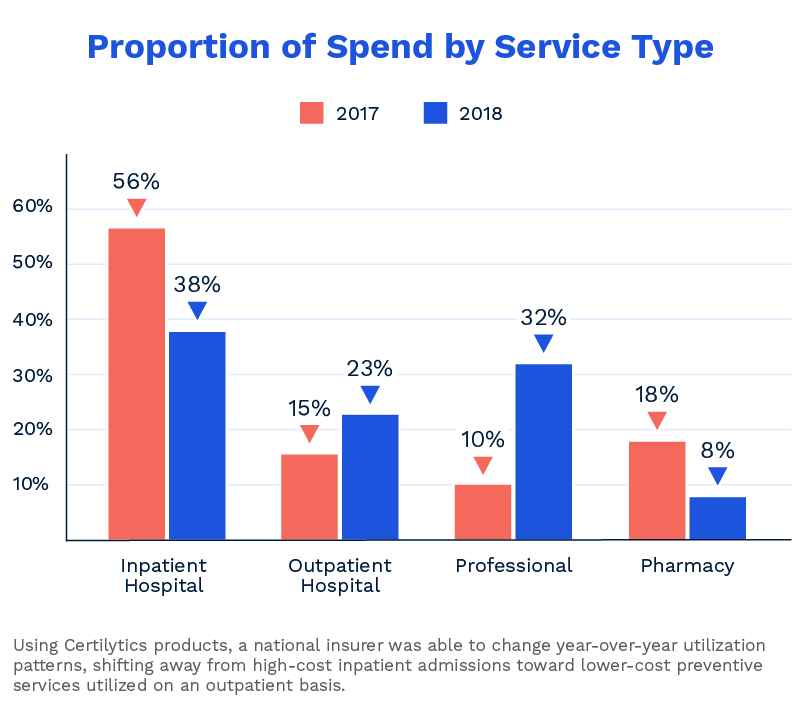
In recent years, healthcare stakeholders have made huge investments in population health management, seeking to improve patient health and lower the cost of care. This blog post explores how one national insurer used Certilytics products to affect positive changes in patient utilization, resulting in millions of dollars in potential annual savings, as the graph below demonstrates.
The Problem
Traditional approaches to population health management typically include identifying patients for intervention based on retrospective factors such as:
- Open Gaps in Care
- Historic Utilization / Costs
- Financial Risk
Unfortunately, these factors fail to provide program managers with a complete picture of their patients’ emerging clinical risk profile. By the time program managers react based on open gaps in care or avoidable utilization, patients have oftentimes already incurred a significant (and avoidable) spike in their healthcare costs.
The Solution
Certilytics enhances the patient identification process with prospective analytics that account for a patient’s likelihood of modifying behavior if targeted by a care manager. Rather than focusing on patients already diagnosed with chronic conditions, Certilytics’ predictive models identify patients at high risk of developing chronic conditions, enabling earlier interventions to prevent high-cost events. These models are aggregated into the Certilytics Health Index (CHI), an AI-powered proprietary algorithm that stratifies patients based on the optimal combination of three factors:
- Emerging Clinical Risk: the prospective likelihood of a patient developing chronic diseases or utilizing high-cost services such as the Emergency Room
- Prospective Financial Risk: a patient’s predicted financial risk over the next twelve months based on medical history, utilization patterns, gaps in care, demographic data, and other non-traditional data sources
- Propensity for engagement: the likelihood a patient will adjust behaviors because of outreach from a nurse or care manager
Because Certilytics’ models account for a patient’s propensity for engagement, Certilytics has a substantial edge over traditional approaches to population health management. For instance, the national insurer found that patients identified by Certilytics as highly likely to engage were 2.6 times likelier to respond to clinical outreach than average.
The Results
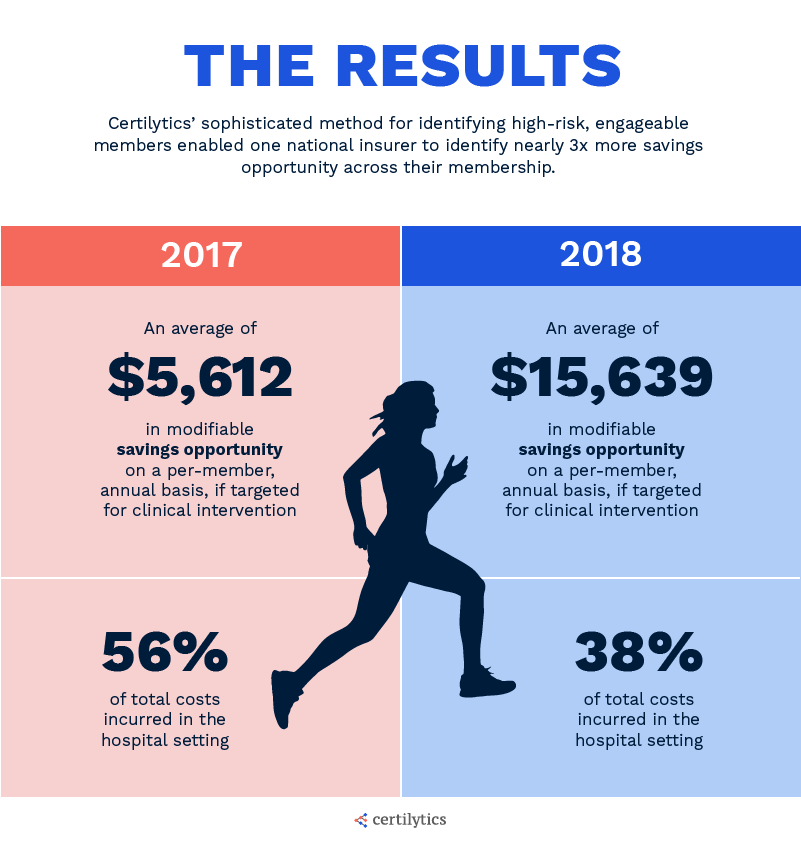
By targeting patients based on prospective measures, including the likelihood of engagement, the national insurer achieved cost savings and improvements in utilization patterns, according to a Certilytics comparison of the riskiest patients from 2017 to the riskiest patients in 2018.
In 2017, when the insurer was using traditional approaches to population health management, the riskiest patients had an average of $5,612 in modifiable savings opportunity on a per-member, annual basis, if targeted for clinical intervention. In 2018, when the insurer was using Certilytics’ approach, the same number of risky patients had an average of $15,639 in modifiable savings opportunity on a per-member, annual basis, if targeted for clinical intervention. The Certilytics approach to population health management resulted in a nearly three-fold increase in identified savings opportunity.
The analysis makes clear that, through Certilytics’ AI-powered population health management products, the insurer did a better job at identifying members with not only the greatest financial exposure but also the members most likely to change their behaviors and prevent high-cost outcomes. Extrapolated to a 10,000-member life group, the Certilytics approach results in millions of dollars in potential annual savings compared to traditional approaches.
The Certilytics approach also had a major, positive impact on utilization patterns. By targeting the patients most likely to engage, the insurer’s clinical intervention efforts succeeded in shifting utilization away from inpatient hospital admissions and toward preventive services such as outpatient PCP visits. As a percentage of total cost per patient, inpatient admissions dropped from 56% in 2017 to 38% in 2018, while spending on more cost-effective outpatient and professional services increased.
To learn more about how Certilytics can help optimize your care management programs, contact us.





