The demand for evidence-based solutions that effectively address Social Determinants of Health (SDoH) has grown. But there’s still not a lot of clarity about which solutions are most effective or the best ways to implement them.
Even though research indicates that SDoH factors can determine up to 80 percent of health outcomes, these factors are often local in nature, making effective responses variable by community and member.
As a result, payers have increased their targeted, local responses, a key piece of which is forging effective partnerships with community-based organizations. In recent years, payer contracts with these organizations have surged.
This type of partnership comes with many benefits. Community-based organizations not only have greater expertise in social health barriers facing the community, but they also have established, trusting relationships with leaders, organizations, and community members.
But finding the right community partner, as well as implementing an effective contract with that organization, remains a complex challenge. On the payer side, the lack of intimate knowledge with a community can hinder the ability to craft realistic objectives, evolve with changing needs, and closely evaluate interventions.
Data-driven insights are often thought of as a first step in learning more about how SDoH factors into a population’s risk. But healthcare leaders are also increasingly leveraging predictive insights to ensure effective partnerships and implement impactful interventions.
Here are three ways forward-looking insights are helping payers like you get the most out of their health equity programs and SDoH partnerships:
1. Drilling Down to Nature of Need
An effective SDoH intervention is one that is tailored to the needs of individual community members or a segment of a population. Understanding and predicting which members carry the most modifiable risk, and which SDoH factors are driving that risk, is a prerequisite to understanding where and what type of SDoH intervention is needed.
Traditional analytic tools that use retrospective analysis may give payers an idea of the level of risk in a population, but not what is driving that risk and how much social health barriers are factoring into that level of risk. This leaves payers without the ability to customize an SDoH intervention and find a partnership that would be most effective.
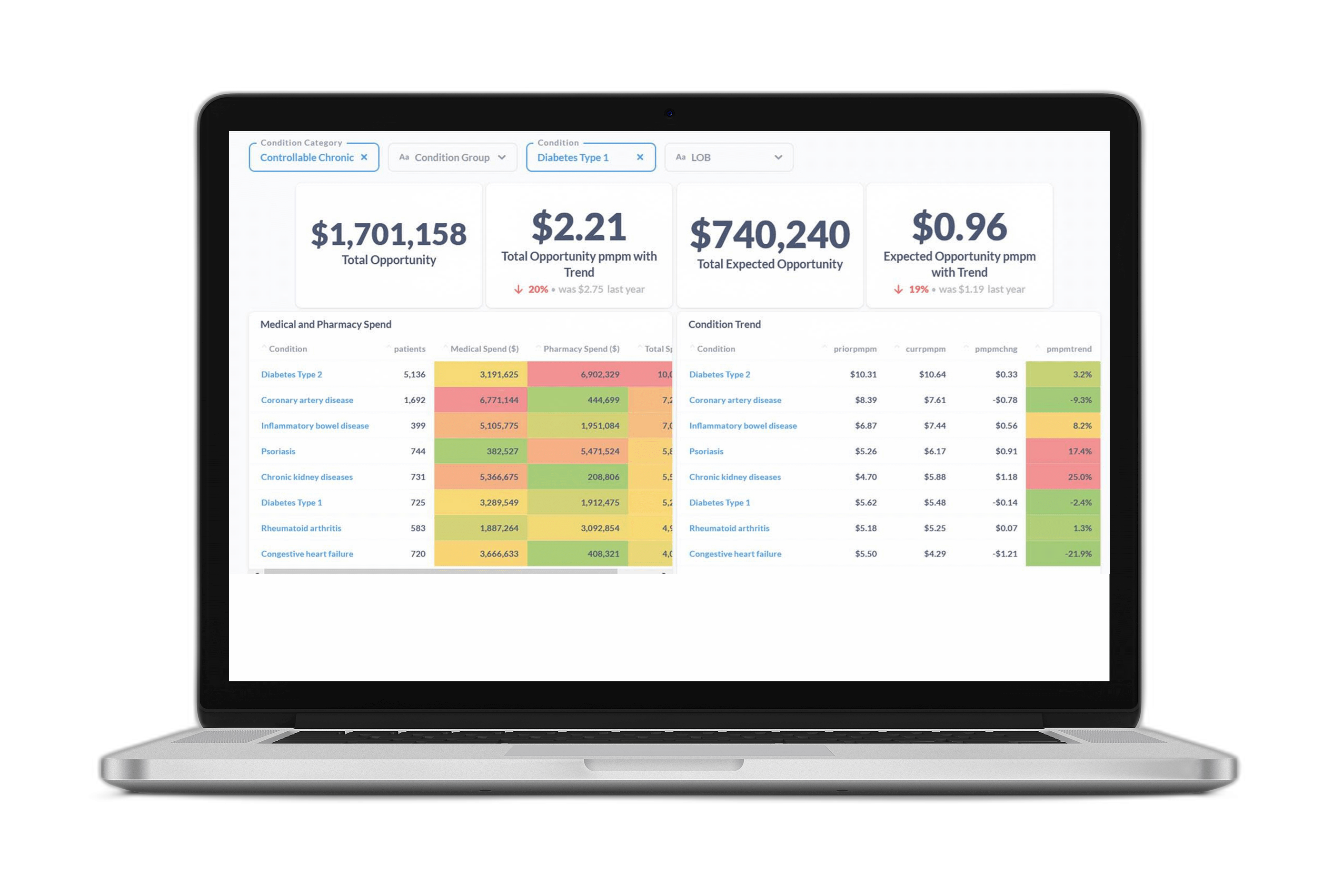
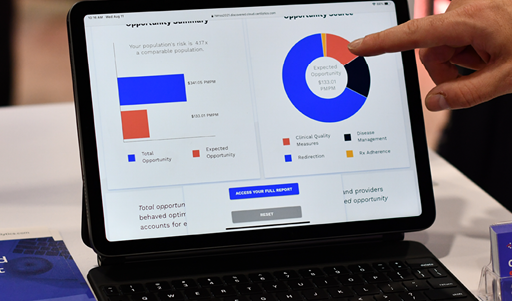
This is why Certilytics built an SDoH predictive model that quantifies and predicts SDoH-derived risk. Our model answers not just the “who” and “where” of SDoH risk, but the “why” and “how.”
These insights enable health plans to prioritize segments of the population for an intervention, pinpointing the geographic area where investment and resources would be best allocated. Payers equipped with this knowledge can precisely narrow their search to a community partner whose location and mission would best support an impactful SDoH intervention.
2. Designing and Developing an Impactful Intervention
Payers rely on community-based organizations for their established connections, but the smaller infrastructure of these organizations also comes with limits.
They can lack the capacity to handle all the needs of a payer’s target population. They also can lack the legal departments and other resources to negotiate and implement value-based contracts with large, nationally-based payers. The pandemic has only worsened this situation for many organizations as staffing and funding shortages have become more frequent.
As a result, it is often left to payers to define the value-based objectives of a contract and strategize the most effective payment models.
Using our SDoH predictive model as well as our data warehousing platform, payers are capable of understanding which SDoH factors have the greatest impact on adverse clinical outcomes for their target population. Our predictive analytics platform also aggregates data from multiple sources to identify those members most likely to engage with outreach.
With this AI-enabled approach, healthcare leaders have the ability to test hypotheses prior to implementing new programs to ensure they are creating real value. They can prioritize outreach initiatives such as educational programs, placement of new clinics, or targeted telehealth outreach.
This allows payers to start a conversation with a community partner with a defined scope for an intervention and the most effective outreach method for different members. Understanding the different levels of risk and propensities to engage allows contract negotiations to adapt and be tailored to a community organization’s abilities, inspiring trust and shared goal-setting among the two parties.
3. Evaluating Outcomes
Too often, payers who have contracted with community-based partners have completed the contracts with more questions than answers. Were the care gaps closed? Which health measures improved? Was the program worth the investment? What changes need to be made to the program to adapt to evolving needs?
Payers need the ability to receive real-time updates on the progress of an initiative to ensure it is meeting objectives.
Our SDoH model and predictive analytics platform provide patient and population-level views of SDoH-derived risk, giving payers updates on changes to an array of health outcomes as well as utilization patterns. This helps payers determine a program’s return on investment and assess what changes, if any, are needed.
If you’re interested in learning more, contact us for a meeting with our team of experts or check out our innovative AI model to predict and quantify SDoH-related risk.