We were delighted to showcase our healthcare predictive analytics solutions at the AHIP 2022 Conference in Las Vegas. Thank you to everyone who visited our booth and attended our bourbon reception.
It was the first time AHIP had held its flagship event in-person since 2019, and a major topic of conversation was the disruptive changes the healthcare industry has experienced as a result of the pandemic. As AHIP President and CEO Matt Eyles put it, “Our healthcare experience has been, and continues to be, reshaped and reconfigured to fit the digital world and the physical world. We don’t always know where one ends and the other begins now.”
Here are Certilytics’ three takeaways from the conference:
1. Telehealth and convenience are now king
Prior to the pandemic, patients were reluctant to utilize services such as telehealth and at-home testing, as Centene CEO Sarah London noted in a panel discussion. But COVID-19 has turned that upside down, with healthcare consumers now demanding convenience.
For the healthcare industry, the key will be building on this momentum as we emerge from the pandemic and ensuring that these services are utilized in the most effective way.
This will require new investments in AI capabilities to enable personalized care strategies that match patients to the right services, treatment pathways, and clinical interventions at the right times.
Many of the healthcare leaders we met agreed that determining a patient’s likelihood of utilizing telehealth services, as well as targeting telehealth services to under-served populations, is paramount to achieving their strategic goals.
Investments in analytic tools that pinpoint the most impactful locations for telehealth services and bridge digital divides are a must-have.
2. Value is more than just a buzzword
For years, value-based care has been a major topic of discussion but difficult to implement in reality for a variety of reasons, including the lack of clearly aligned priorities between payers and providers.
But, as London explained in her panel discussion, the pandemic was an inflection point. Utilization rates plummeted as patients avoided healthcare facilities and postponed preventive care—forcing payers and providers to come together to focus on whole-person health.
The transition from fee-for-service to value-based care is leading to innovative shared-risk arrangements where both payers and providers have a financial stake in improving health and managing costs. This is driving a major shift in population health management.
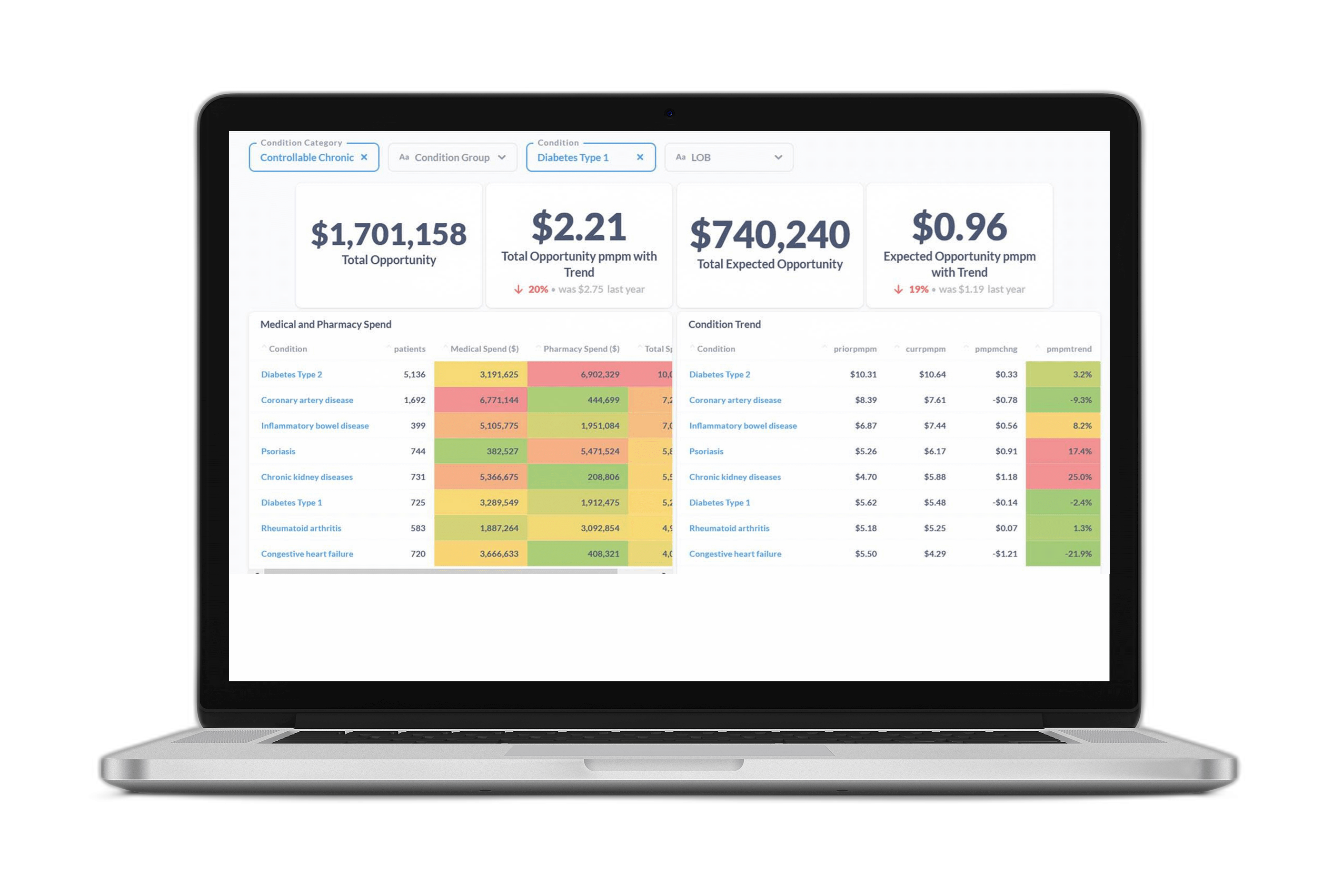
Traditional, retrospective analytic tools were built to serve the fee-for-service model—and they ignore the fact that the highest-cost members aren’t always the ones who will benefit most from clinical intervention. A member with lower overall financial risk—but more open care gaps or redirection opportunities—might be a better candidate for outreach, especially if the member shows a high propensity for engagement.
As healthcare organizations transition to value-based care, they’re moving toward prospective reporting that predicts not just risk, but modifiable risk, as we do through the Certilytics Opportunity Framework. This is the best way to reach members before they incur avoidable, exorbitant costs—and unlock true value.
3. We all have data—the challenge is connecting it
A number of panelists noted the importance of incorporating more data sources—beyond just medical and pharmacy claims—and connecting everything on one platform to produce a clear, transparent view of patient and population health.
As several speakers mentioned, robust analytic tools capable of connecting the vast array of data sources from both inside and outside the clinician’s office – especially social determinants of health factors – is critical to these efforts.
It’s why more healthcare organizations are turning to data management tools that produce a holistic, forward-looking views of member and patient health—with AI-powered enrichment’s that enable advanced predictive analytics.
Not only that, but healthcare organizations are increasingly demanding customizable tools that meet their specific clinical and business needs, allowing them to build their own reports and visualizations and answer their most pressing analytic questions.
Thanks again to all those who made time to connect with us in Las Vegas—we hope to see you again (or for the first time) at next year’s conference!
To learn more about how Certilytics can help you win and retain business contact us for a product demonstration or to meet with our team of experts.