As a benefit leader, you understand the promise offered by specialty drugs for employees and their families.
You’re also well aware of how specialty drugs contribute to surging healthcare costs.
The question is how best to manage the costs and complexities of specialty drugs – so you can continue to meet your goals of improving employee health and well-being, strengthening recruiting and retention, and ensuring the smartest healthcare spend possible this year and in years to come.
Getting a Handle on the Medications, the Care Setting, and How Both Impact Outcomes & Costs
Today, specialty drugs make up half of all U.S. pharmaceutical spending, split more or less equally across medical and pharmacy benefits.
At the individual level, discerning why one care setting or specialty drug is more appropriate than another becomes far more difficult. As a benefit leader, your job is to make sure your health plan partners and vendors are looking at the whole picture—and taking steps to ensure the right specialty drugs are being administered in the right setting.
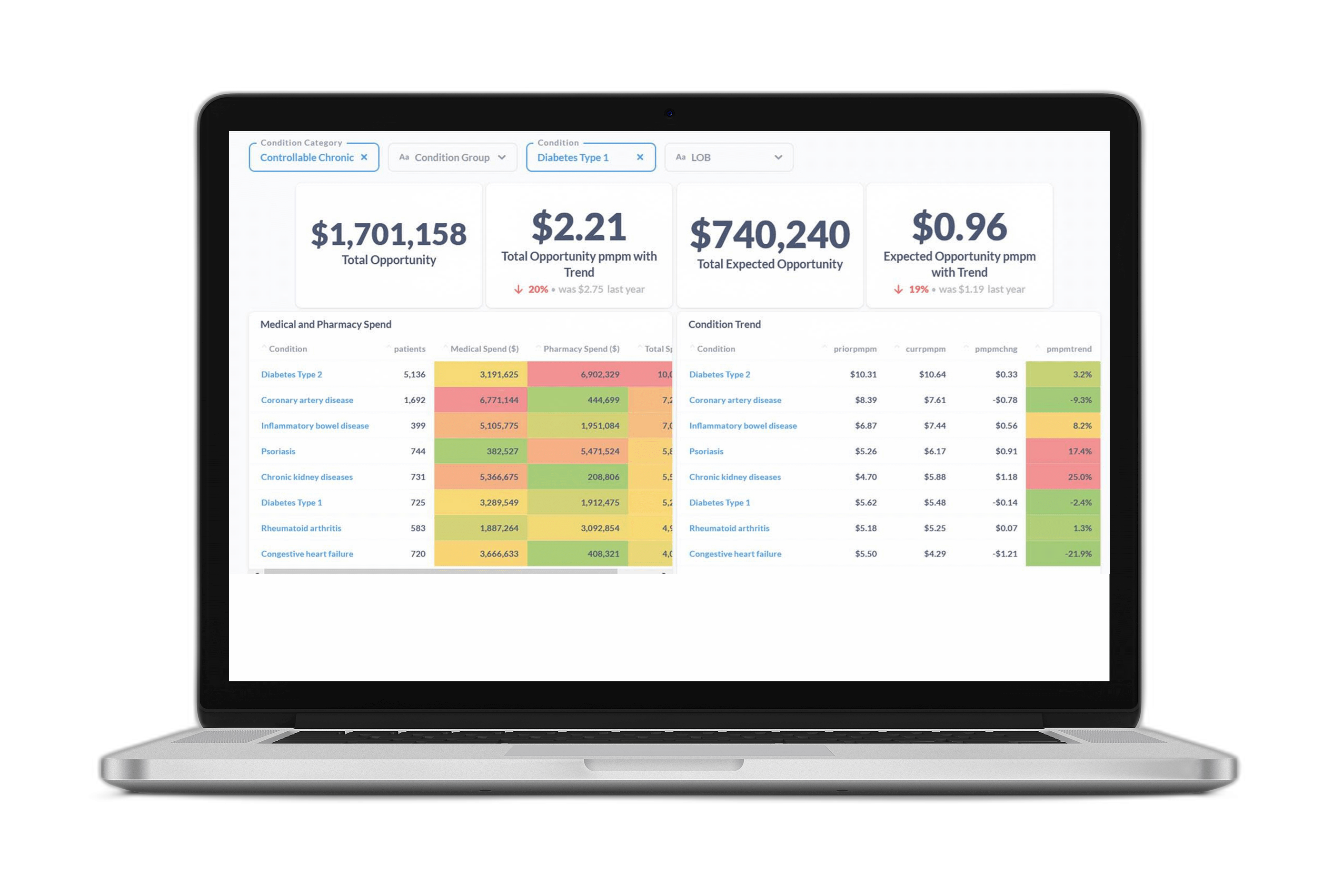
This means viewing the complexities of specialty drug spending through a connected lens of cross-benefit analysis and integrated pharmacy reporting. Your data partners need to be able to connect medical and pharmacy claims on one platform to enable “whole person” health analysis. This will allow you to pinpoint cost savings opportunities today that improve member health and well-being tomorrow.
Clear reporting that puts the answers at your fingertips also gives you a way to help other senior leaders understand the difference between smart spending and avoidable overspending. You can quickly show your company’s executives the full, positive impact of programs and decisions rather than having to manually pull and reconcile disparate reports.
Managing Specialty Drugs Shouldn’t Feel Piecemeal or Reactionary
The most sophisticated analytics and reporting tools also have future cost and utilization predictions baked into the reports – so you can see an accurate forecast of how specialty drugs currently in the FDA approval pipeline will impact members’ health, well-being, and pharmacy-related spending across benefits.
Accurately predicting the financial and clinical impact of specialty drugs in the FDA approval pipeline is critical to long term benefit strategy & plan design. In 2019 alone, two-thirds of the novel therapies approved by the FDA were specialty drugs – and nearly 60% of the drugs awaiting approval through the end of this year are also classified as specialty pharmaceuticals. So the need to understand and nimbly manage specialty drugs across benefits will only increase in the years ahead.
By seeing your plan members’ whole health through a connected lens that includes current and future specialty drug utilization, you can further ensure your integrated pharmacy spending and strategy supports the health & well-being of employees and their families to the fullest degree possible. Because, after all – that’s what your employees are counting on you to do.
Ready to learn more? Check out how you can Build a Smarter Benefits Plan with Certilytics.