The new price transparency regulations promise unprecedented competitive intelligence for health plans, but the machine-readable files in which they are packaged come with some major data obstacles.
With the help of an experienced analytics partner, health plans can access actionable data insights from these files that give their teams an edge in a highly competitive market. What are some of the most effective ways health plans can use this intelligence?
Here are three ways our health plan partners leveraged price transparency data insights from Certilytics’ data analytics platform and turned their competitive intelligence into a competitive advantage.
Use Case #1: Access to Competitive Pricing Analysis
One of our health plan customers wanted to use the price transparency data to compare their rates with a competitor. This Midwest-based health plan wanted to identify trends and spot price variations so they could make impactful rate adjustments.
But once they gained accessed to the files, they quickly realized that drilling down into price variance across different services, price bundles, and locations was going to require data expertise.
Why? The files are massive, requiring a technological platform capable of ingesting terabytes of data. In addition, there’s no standardization in the files. For example, information on one plan could be spread across multiple files or one file could contain multiple rates.
In order to even begin a pricing comparison, the health plan analytic teams needed to overcome the technological hurdle of consuming massive amounts of data and de-tangle the data enough to understand which product and network related to which file.
Certilytics’ data analytics platform not only aggregated the enormous amount of data, but normalized it into one consistent layer and enriched it with supplemental provider and COB data.
This linked group practices and health systems together in order to compare the fees the carriers supplied in the price transparency files to Certilytics’ and COB’s reference database of millions of providers. This extra step validated the accuracy of the figures supplied by the carriers so that the health plan could be sure they were working from precise numbers.
Once the data was validated, cleansed, and ready for analysis, our platform also saved the health plan time and resources by supplying insights through intuitive reports and dashboards.
With quick, reliable insights at their fingertips, the health plan teams explored a summary of competitor network fee schedules across inpatient, outpatient, and professional service categories as well as accessed the source MRF datasets. Plus, the reports include Medicare and the client’s reimbursement levels for straightforward bench-marking.
In the end, Certilytics’ data insights helped the health plan analytic teams compare their plan’s pricing, networks, and rate file completeness with multiple other plans, broadening the scope of their initial analysis and informing their pricing strategies.
Use Case #2: Strengthen Negotiating Power in Provider Contracting Efforts.
For another Midwest-based health plan partner, the price transparency files gave them the unprecedented opportunity to compare provider reimbursement rates, specifically which providers were offering their competitors lower prices. In this case, the health plan team wanted to analyze the fees from a provider in a rural hospital.
But again, the enormity of the files and their lack of standardization made drilling down to this one provider much like finding a needle in a haystack.
Within the files, multiple providers could be associated with one national plan that has filed their information nationally, making a rate comparison in a local market time consuming. Incomplete information also existed in the price transparency files. In the example below, the internal provider group ID came with no corresponding lookup information and with thousands of nested NPI’s.
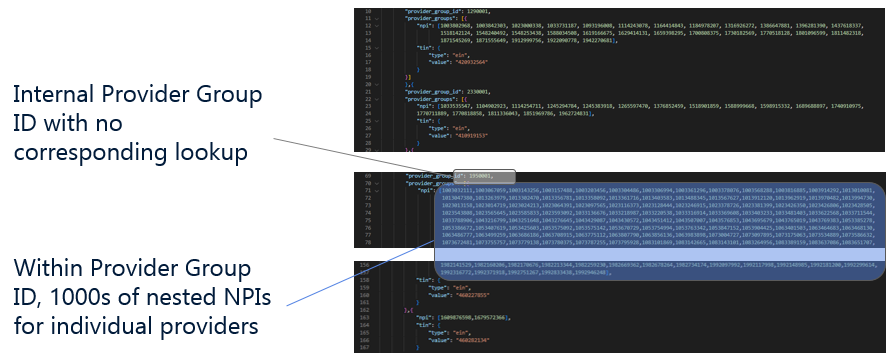
In this instance, they were therefore presented with very little information about this provider group and must grapple with the fact that every rate for the provider group ID is mapped to multiple providers, regardless of the fact that many of the individual providers don’t fulfill the type of service in question.
On top of a lack of consistency in the provided rates, there was no comparison to Medicare, making any basis for a reasonable assessment of one reimbursement fee impossible from the raw data.
Certilytics’ aggregated, standardized, cleansed and linked the files to reference databases to create the most holistic cost analysis possible. By supplementing the data with Certilytics’ provider database and COB’s database, Certilytics’ platform caught a price discrepancy that would’ve thrown off the health plan’s analysis.
The result? The health plan now had the ability to drill down to one provider in a rural hospital and analyze the reimbursement fees.
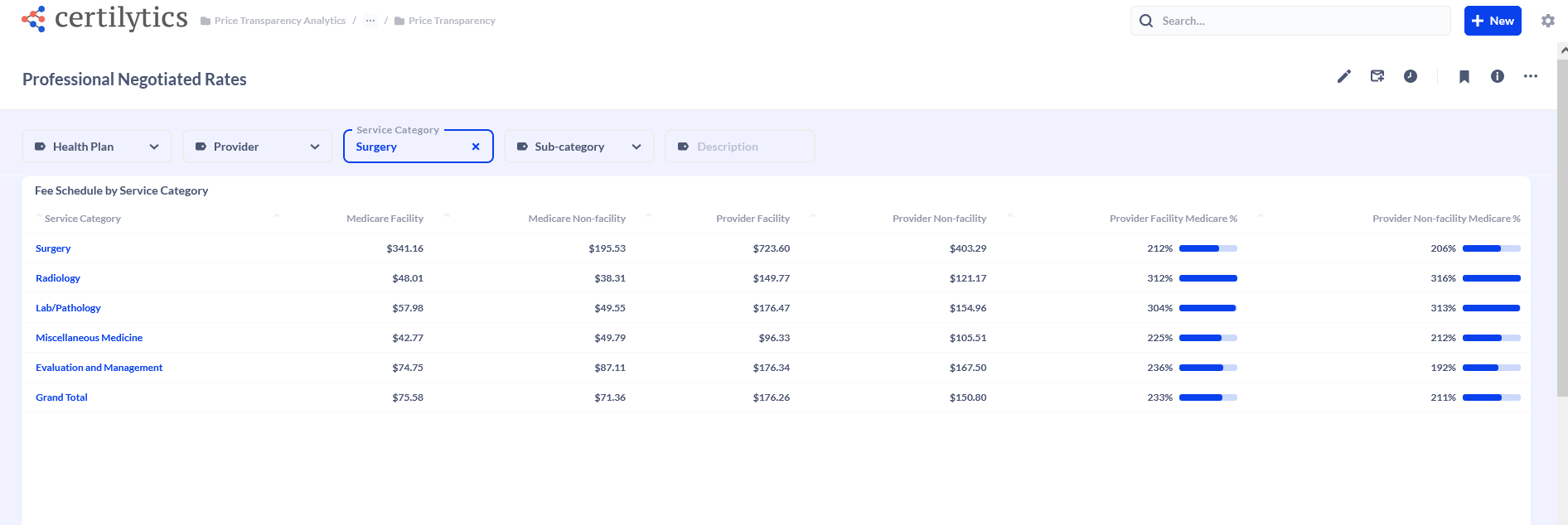 Professional Rates
Professional Rates
Using this insight, health plan leaders acquired the ability to secure a more desired contract with an in-demand provider.
Use Case #3: Develop Strategies to Win and Retain Business with Employer Clients.
For our third use case, a Southwest-based health plan partner sought a competitive advantage from the price transparency files when it came to acquiring and retaining employer clients in a specific market.
They were looking for different answers from the data, but they ran into the same obstacles as our other health plan partners. Without the help of Certilytics’ data platform, a pricing analysis of rate structures and provider reimbursement fees wasn’t possible.
Provider lookup information was incomplete or scattered across multiple files. The same was true for competitor rates, with information on one plan spread across multiple files or one file containing multiple rates. National plans that filed nationally were difficult to analyze on a local level.
And on top of the sheer volume of the data, the accuracy of the numbers remained a concern without a reference database like Certilytics’ provider database, which contains the fee schedules of millions of providers, to validate the figures.
Certilytics’ platform performed the heavy lifting of aggregating, standardizing, cleansing, and validating the data to make a price comparative analysis possible. The health plan could then explore a summary of competitor network fee schedules across inpatient, outpatient, and professional service categories, access the source MRF datasets, and benchmark their reimbursement levels against Medicare.
In the end, this health plan understood which of their employer clients may be at risk based on pricing, and could adjust offerings to retain that business.
They also gained insight into new employers in that local market who would be better served by their health plan offerings.
Ready to see how you could turn competitive intelligence into your next competitive edge? Meet with our team to see how you can leverage your price transparency insights.





