Certilytics has been an AI and machine learning company since day one because we believed unified data and AI-driven predictive analytics have the power to keep people healthier and make healthcare more affordable.
For more than 11 years, leading healthcare leaders have chosen to embrace our AI-driven solutions because they were tired of relying on retrospective data and insights which were making it impossible for them to break the endless cycle of increased costs and poor outcomes.
Through these partnerships, we have seen the significant impact our AI-driven predictive analytics are making on how quickly organizations can go from data to action. That’s why we’re introducing Benefit Intelligence, a new and first of its kind solution to the employee benefit space because everyone deserves a chance to pay less for healthcare and live healthier lives.
Here are the top 3 reasons our team has dedicated our efforts to delivering an innovative AI-powered, game-changing solution for benefit leaders:
The Need for Benefit Leaders to Make Data-Driven Decisions Faster
Like never before, employers have access to a lot of data on their employees and their interactions with the healthcare system. We all know within this data lives valuable insights, but the process of collecting the data and turning into actionable intelligence can prove difficult.
Today, most benefit leaders work with a data and analytics partner who is collecting their data, but they are only giving them access to the raw data, which only provides retrospective analytics.
To get ahead of rising costs and poor outcomes, benefit leaders need to switch to a predictive analytics strategy.
With Benefit Intelligence, our AI-driven approach to collecting and enriching data and delivering forward-looking insights can improve your time from data to being able to make confident, benefit plan decisions.
Using AI, we can quickly ingest your raw data, enrich it using our library of 1,000+ predictive models and deliver predictive intelligence. Here’s a dashboard of our Opportunity Analyzer, where benefit leaders can identify future health risks within a population and see in dollars where there are the largest opportunities for cost savings.
Opportunity Analyzer

The Growing Demand for Cost Cutting Solutions
As healthcare costs continue to rise, benefit leaders are under pressure to find ways to reduce healthcare expenses. With no control over what’s happened in the past, the only way to cut costs is by predicting what costs may be incurred in the future.
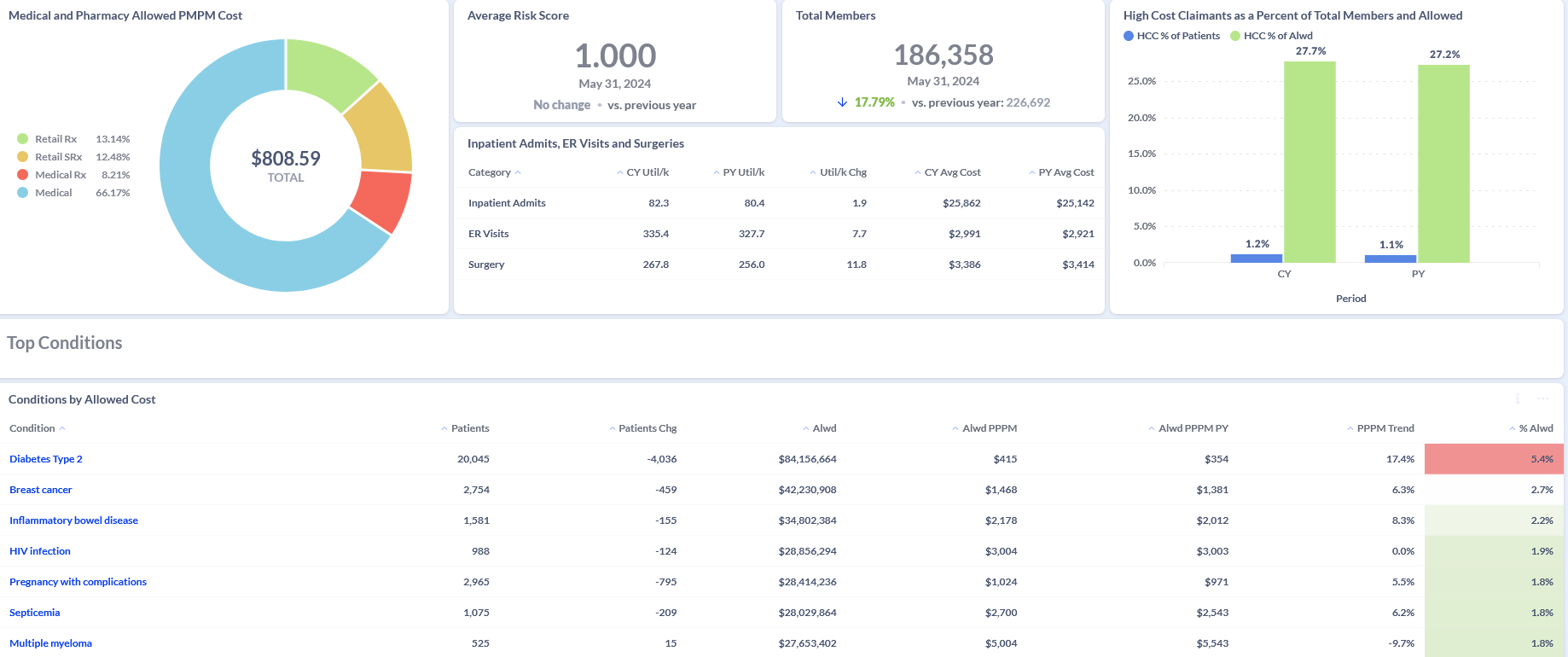
With Benefit Intelligence predictive intelligence, you can identify cost savings by better anticipating your high-cost claimants with our High Cost Claimants Analyzer. And, with the Condition Analyzer, you can better understand where the largest savings opportunities exist and then redirect members to another service or pharmaceutical intervention that can reduce overall spend.
High Cost Claimant Analyzer

Condition Analyzer
The Increased Pressure to Prove Value and ROI of Programs & Strategies
As a way to better manage costs and improve outcomes, most benefit leaders have embraced working with healthcare management solutions. These solutions can be expensive, but they promise to deliver results. Yet, many benefit leaders are left questioning whether or not these programs are delivering value.
With Benefit Intelligence, we use a proven and unique AI-driven approach to measuring ROI of these vendors. Using the Impact Analyzer we can calculate the total realized cost savings associated with each existing program or strategy, including an ROI analysis of the actual costs compared to costs without the program.
Impact Analyzer

By embracing our AI-driven approach, one Fortune 50 employer has already identified $70.6M in total savings opportunity and achieved $36,443,000 million dollars in cost savings to date. If you would like to achieve these kinds of results, reach out to our team to learn more about Benefit Intelligence.









